Two sides, same coin.
Therapy & medication in one place.
Studies show that the combination of medication and psychotherapy is better than either one alone.
Simply taking medication doesn’t shift the psychological patterns underneath symptoms of depression, anxiety, and trauma. But psychotherapy alone sometimes cannot gain traction when the symptom load is too high. Together, these modalities compliment each other, with medication supporting the conditions where insight can take root and heal the psyche at a fundamental level. (Cuijpers 2020, Pampallona 2004)
Therapy for all!
Therapy transformed my life. I want that for you, too.
We all need someone outside of our own mind, outside of our day-to-day family and social sphere, to help us see our own life clearly. Our usual patterns, developed for our own safety in childhood, are so ingrained, so reflexive that they are almost impossible to notice, let alone change once we outgrow them.
Therapy has given me so much more spaciousness in my mind and behaviors, freed me from old conditioning so that I could choose the life I actually want. It is my goal to create the right emotional container—full of trust, insight, respect, and humor—for you to do the same thing in your own way.
What are the advantages of combined treatment?
-
Rather than having separate appointments for medication and therapy and hoping those people talk to each other, you can consolidate your treatment with one person. One payment, one system, one time signing all the annoying paperwork. I’m happy to coordinate with your primary care doctor or another important person or provider.
-
It is possible prescribe effectively to people I do not see for therapy, but if I’m meeting with you weekly and learning about the nuances of your symptoms and experiences, I can see things I wouldn’t otherwise, and the medications can be adjusted more responsively. It is the opposite of prescribing by checklist.
-
Treatment is more than the sum of its parts; the various aspects amplify each other. Medication helps therapy work better, and therapy helps medication work better. Just like mind and body aren’t separate, neither are therapy and medication. It’s a unified approach so it can be nice to have it all “under one roof.” Medication can become a topic of therapy itself—you may have complex feelings about taking it, and you may have had negative experiences with medication or psychiatrists in the past that need to be understood.
-
There are so many options. Therapy without meds. Meds without therapy. Therapy and meds both with me. Meds with me and therapy with another therapist. You don’t have to fit in a predetermined box; rather, we can tailor the treatment to fit you and your preferences.
Are MD psychiatrists really trained to do therapy?
Good question. Psychiatry as a field has moved away from psychotherapy to focus on medication and technological interventions. But psychotherapy has always been a mainstay of psychiatry, and I still see it as the heart of mental health treatment.
I chose my residency program specifically because they emphasized training in psychotherapy alongside psychopharmacology. We started seeing therapy patients in our second year and worked one-on-one with supervisors to guide our development as therapists. My fourth year, I spent two days a week training at the San Francisco Jung Institute.
After completing residency, I joined a group practice dedicated to giving psychiatrists the opportunity to offer psychotherapy. We had monthly case consultation, semi-annual in-depth trainings, and a community of like-minded physicians who valued therapy. My 11 years with that group solidified my practice combining medication and therapy, and I can’t imagine working any other way.
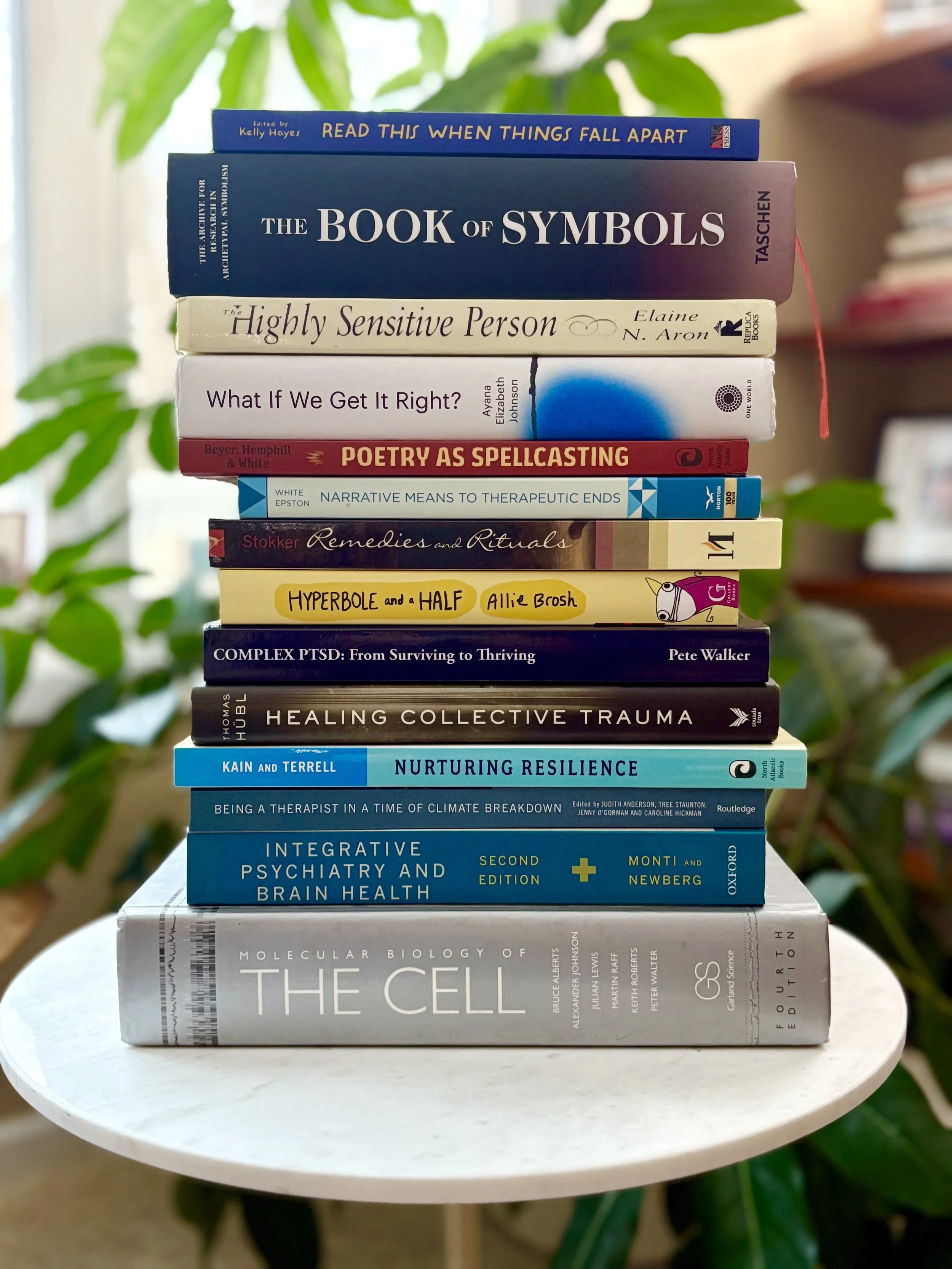
Now in private practice, I continue to seek out ongoing consultation, education, and colleague support to grow as a multi-faceted clinician. One of the best parts of my job is that I never stop learning, and I get to apply what I learn in the service of healing.
My psychotherapy approach
-
So much of how we feel is based on the stories we tell ourselves about what happened and why. But there are multiple ways to tell a valid story about the same events. One aspect of psychotherapy is questioning our current stories and exploring alternatives. When we update the narrative around traumas, we don’t erase them, but we carry them differently. Some stories feel so shameful they have never been shared. I hope to create a space where the unspoken can be spoken so that you’re supported and not alone with it anymore.
-
Life comes with some real concerns about how to live meaningfully. How do we go about our day knowing that life is unpredictable? Therapy can be a place to explore human dilemmas around the nature of existence. Smaller anxieties are often related to larger anxieties about life and death, what it means to be human, how to cope with rapid change in modern society, and our inherent lack of control. I don’t shy away from this level. Even though we don’t exactly answer these questions, addressing them directly, and together, can make them more manageable.
-
Too often, the mental health field pathologizes individuals instead of naming societal ills. The lens of liberation psychology considers social justice aspects of well-being. If you feel like you are failing at work, we consider what it takes to succeed within late capitalism. If you have social anxiety, we look at the ways race and identity might be at play in the difficult interactions. We wonder whether travel stress is connected to climate/carbon concerns. Seeing that it’s not “just you” can alleviate guilt and shame.
I also bring an awareness of the power dynamic between the two of us in the therapy itself, and I actively welcome your feedback on how I’m showing up.
-
Not all trauma is overt, like physical abuse or car accidents. Most people carry some subtle form of trauma — such as emotional neglect, microaggressions, or immature parents — that they are holding in their psyches and their bodies. When these layers can be identified and worked through, they deliver profound lessons and free up new stores of energy.
-
Humor is the spoon full of sugar that makes the trauma-processing go down. If we can laugh together, healing is happening. We can all use some well-timed lightness to balance the heavy topics, right? I don’t joke around to avoid the pain; rather, I see shared humor as connection, safety, and perspective.
My prescribing style:
Gentle
Many people have had bad past experiences with medications because their doctor started too high, increased too fast, or overlooked interactions. I want you to feel safe and secure as you embark on a new medication. Let’s be honest, it’s kind of nerve-racking to alter your brain chemistry. I do everything I can to help you feel informed, prepared, and held, with your questions answered and doubts addressed as much as possible.
Effective
There is no point to taking medication that doesn’t work. I meet way too many people who feel “meh” about their meds, like “maybe” they are helping. We can do better than that. I want you to think they are awesome. I want you to look forward to taking them. I want you to notice real benefit in your daily life. We don’t have to settle for so-so, or tolerate side effects that get in the way of enjoying life.
Creative
Prescribing is both a science and an art. I combine rigorous knowledge of psychopharmacology with intuition and pattern recognition I’ve developed over the last 15 years of practice. The way bupropion works for certain flavors of low motivation, lamotrigine works when “depression” has a subtle whiff of bipolar, and a selegiline patch works when nothing else has. Having supplement, herbs, and HRT at my disposal rounds out the toolbox in a way that is flexible and effective.
Collaborative
Sure, I’m the one who went to medical school, but you are the one taking the medication. My ideas are only as good as your enthusiasm about them. I never want you to feel pressured into taking medication, by me or anyone else. Sometimes people tell me, “They said that [insert side effect here] can’t be a side effect of the medication.” Virtually anything can be a side effect of any medication, so I always take it seriously if something crops up when you start a new med.
Responsive
At first, medications require tweaking. I am available to help make the small adjustments that matter. I tell my patients to have a low bar for getting in touch if something is concerning them about their meds. You shouldn’t have to wait for weeks (or months) for changes. Responsive also means knowing if and when to consider stopping meds; I attune to shifts in your psychology and behavior over time that could signal a moment to carefully reduce your dose and potentially go off.
Placebo-friendly
Every few years, a news story runs decrying that psych meds are no better than placebo. My takeaway isn’t to forsake medication but rather embrace placebo. Psychiatric medications work on the physical, material level, altering neurotransmitter levels and modulating synaptic transmission. And they also function as potent symbols, imbued with cultural power and belief, operating on an emergent level as well. Rather than deny placebo effect, I do everything I can to enhance it.
You can have a one-stop shop for mental health care.
Click here to set up an introductory call, whether you want medication, therapy, or both.